A Guide to learn about the best Treatments for Keratoconus
- Apr 10, 2024
- 4 min read
When it comes to the health of our eyes, we often take our vision for granted. We never stop to think when the situation might change for our eyes. Keratoconus is a progressive eye disorder that significantly alters an individual’s visual abilities. But for those who suffer from a condition called Keratoconus, daily life can be a constant struggle. In the first part of our article, we'll delve into what Keratoconus is, its causes, and the symptoms it presents.
Let’s start with the basics
What is Keratoconus?
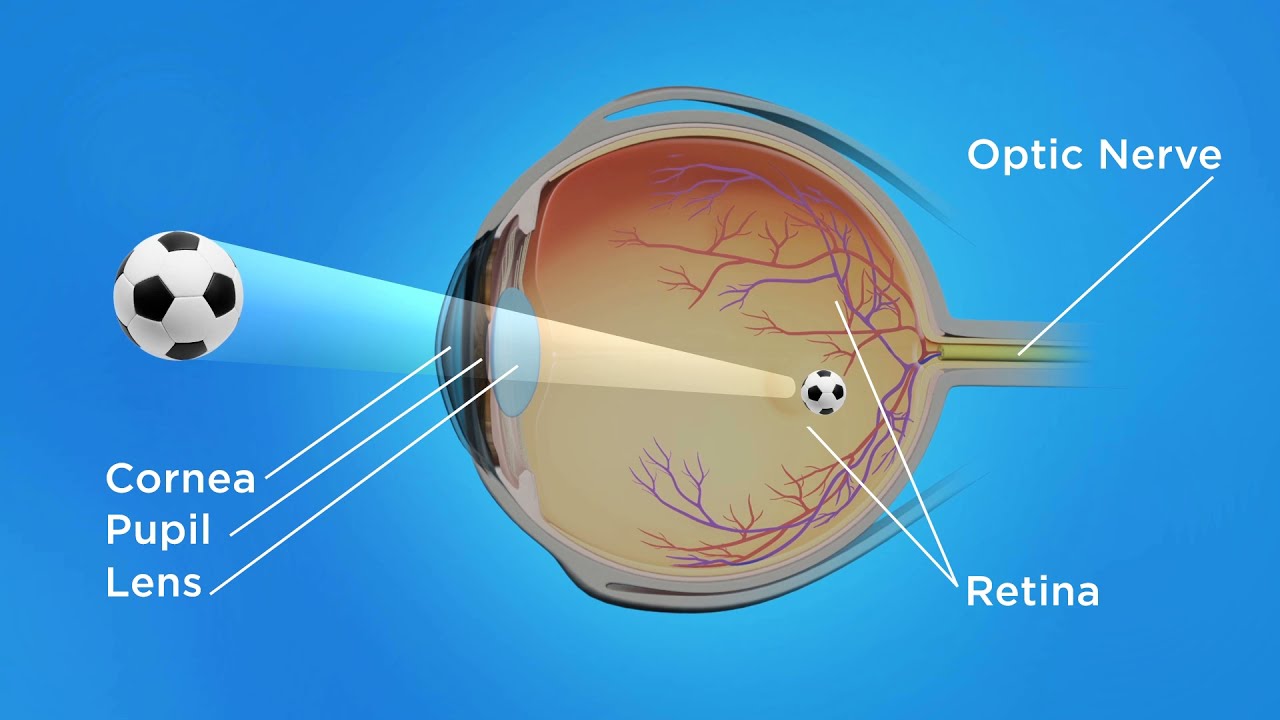
Keratoconus (K’Conus) is a condition with progressive, non-inflammatory bilateral corneal ectasia, affecting one eye more than the other. It manifests with a characteristic cone-like steepening of the cornea associated with irregular stromal thinning, resulting in a cone-like protrusion and significant loss of vision.

What causes Keratoconus?
The interplay of genetic predispositions and environmental triggers in the diagnosis and treatment of Keratoconus is undetermined and a subject of ongoing research. Studies are exploring genetic markers associated with the condition, alongside external factors such as ultraviolet exposure and allergens, aiming to uncover prevention and early detection strategies.
Yet, several associations have been identified, which include rubbing of the eye, Down Syndrome, Atopic Disease, Connective Tissue Disease, and genetic disposition.
What are the first clinical signs of Keratoconus?
The first symptoms of Keratoconus appear during puberty or late teens. Symptoms usually look like blurred vision, sensitivity to light and glare, double vision/distorted vision, and constant itching and rubbing of the eyes.
It is often accompanied by significant Myopia, irregular corneal astigmatism & stromal thinning.
The corneal thinning and the asymmetric astigmatism both occur in the area of the corneal protrusion, which is often inferotemporal.
The Clinical Evaluation of Keratoconus
Corneal Topography and Pachymetry are the prime diagnostics used in the diagnosis and evaluation of Keratoconus in addition to slit-lamp bi-microscope evaluation.
Corneal Topography

Pachymetry


Back in the day, as old as the 1800s, a Placido’s Disc was used to detect irregular corneal astigmatism.


What are the treatments available for Keratoconus?
The available treatments are highly dependent on the stage of the condition and its progression. If the condition is stabilised (non-progressive), it is corrected by Sphero-Cylindrical Correction in the form of eyeglasses which can also improve vision.
Non-Surgical Solutions for Treating and Managing Keratoconus
If the condition is progressive, the emphasis is to slow down (arrest) the progression by RGP Contact lenses, Keratoconus lenses (Rose-K, Accucone contact lenses), and Scleral contact lenses.
Advanced Contact Lens Treatments

Rigid Gas Permeable (RGP) Lenses
As Keratoconus advances, achieving clear vision with standard eyeglasses or soft contact lenses becomes increasingly difficult. Rigid Gas Permeable (RGP) lenses are a vital treatment option, providing a durable and consistent vision correction alternative. Specially designed lenses, like Rose-K and Accucone-K, are crafted using digital processes to ensure a perfect fit, accommodating the cornea's irregular shape with precision.

Scleral Lenses
For those seeking further comfort and clarity, Scleral lenses are another option in the treatment of Keratoconus. These larger lenses rest on the white part of the eye (the sclera) and vault over the cornea, creating a fluid-filled chamber that corrects vision by smoothing out irregularities and providing hydration to the corneal surface.
C3R Procedure
If the keratoconus is progressing, Corneal Collagen Cross-Linking(C3R Procedure) may be indicated to slow it down or prevent it from getting worse. C3R is a non-surgical treatment but is classified as a procedure as it takes place in the operation theatre.

Surgical Management of Keratoconus
You may need surgery if you have corneal scarring, extreme thinning of your cornea, poor vision with the strongest prescription lenses, or an inability to wear any type of contact lenses.
Depending on the location of the bulging of the cone and the severity of your condition, surgical options include:
Intrastromal Corneal Ring Segments (ICRS)
For mild to moderate keratoconus, your eye doctor may recommend inserting small synthetic rings in your cornea. This treatment can help flatten the cornea, which can help improve vision and make contact lenses fit better. Sometimes, this procedure is done in combination with corneal cross-linking.

Cornea Transplant
If you have corneal scarring or extreme thinning, you'll likely need a cornea transplant. Depending on your situation, your eye doctor may recommend replacing the whole or part of your cornea with a healthy donor tissue. A cornea transplant is also known as a keratoplasty.

Early diagnosis helps prevent the condition from worsening.
The Critical Role of Regular Eye Exams
Stressing the importance of regular comprehensive eye exams for early detection and intervention of Keratoconus can lead to better treatment outcomes, emphasising the necessity of these eye examinations in identifying early signs of the condition.
The Psychological Impact of Keratoconus
The emotional and psychological challenges of living with Keratoconus can be significant. Addressing the impact on daily life, social interactions, and mental health, alongside resources for psychological support, is crucial for comprehensive care.
Living with Keratoconus can be daunting, but understanding the condition and the available treatments can transform the outlook for those affected. From spectacle lenses to advanced RGP and Scleral lenses, a variety of solutions exist to combat the challenges posed by this eye disorder. With ongoing advancements in the Keratoconus eye condition treatment, patients have access to cutting-edge options that can lead to significant improvements in vision and quality of life.
The journey through diagnosis and treatment requires patience and a proactive approach to eye health. By staying informed and working closely with eye care professionals, individuals with Keratoconus can navigate their condition more effectively, embracing clearer and brighter vision.
Keratoconus presents a unique set of challenges, but with the right approach and access to modern treatments, it's possible to manage the condition successfully.
Want to know how to prevent, manage and treat Keratoconus? Book an appointment with our optometrists today!

































Comments